Project
Bump2Baby and Me is a five-year project to develop and evaluate an innovative healthcare intervention to help prevent maternal and child diabetes, overweight and obesity and other non-communicable associated diseases.
Why does it matter?
Gestational diabetes is a growing burden worldwide and has a significant impact on health services. Around one in eight pregnant women will experience gestational diabetes. This can seriously affect the future health of women and their children.
Our research
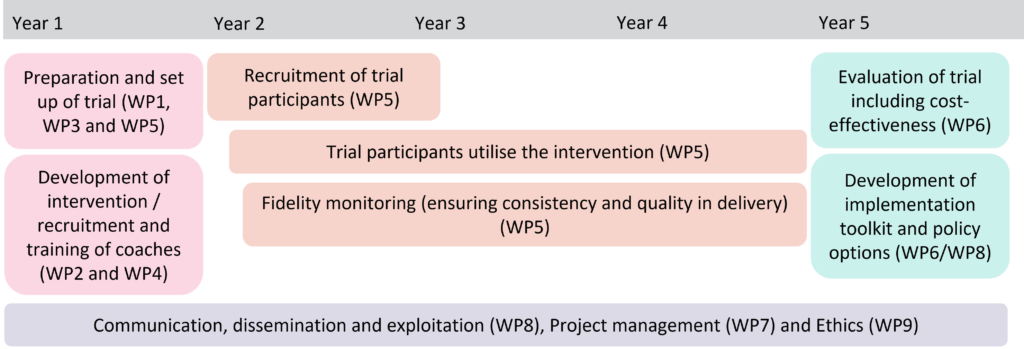
Our research is split into nine work packages (WPs), designed to specifically meet the project’s objectives.
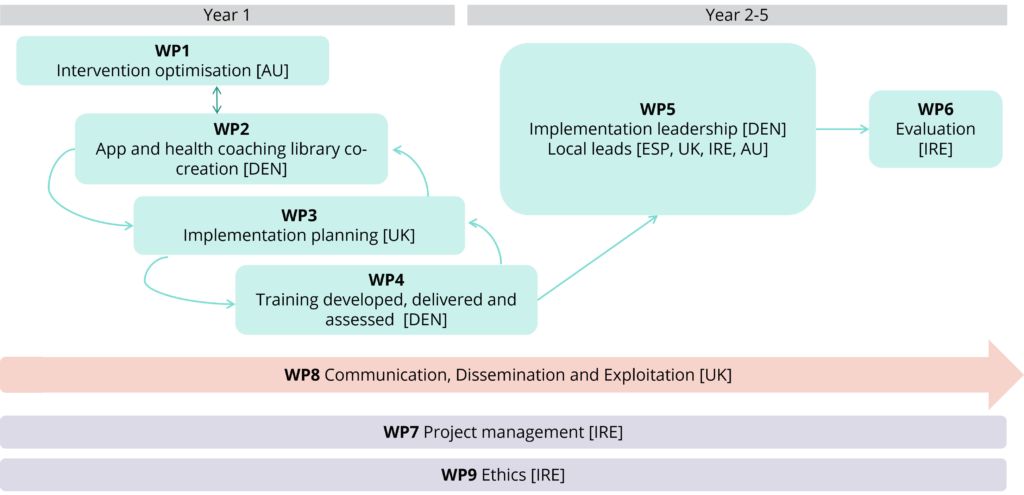
This work package will perform a systematic scoping review to identify and deconstruct effective interventions, including examining the cost effectiveness of the interventions. The review will consider other apps or programmes which are already in the marketplace and develop an understanding of how they have been implemented and how effective they are. This work will guide the mapping and classification of behaviour change to enable the development of an optimised framework for postnatal intervention.
Partners involved: Monash University (Lead), University College Dublin, University of Copenhagen.
Work package 2’s main output will be to deliver a tailored and co-created Bump2Baby and Me app in both English and Spanish. The co-creation will be done with input from key stakeholders in each country (Australia, Ireland, Spain, and UK). The app will include content and a health coach manual, and inter-country differences such as guidelines and local practices.
Partners involved: Liva Healthcare (Lead), Aarhus University, Monash University, University of Bristol, University of Copenhagen, University of Granada.
The objectives of work package 3 are to identify and map the external contextual factors that influence both gestational weight gain and gestational diabetes (GDM) management for each trial site; and to identify the use of GDM risk screening tools and GDM mHealth technology across each site.
Information from work package 1 will guide the mapping work and this work will inform work packages 4 and 5.
Partners involved: University of Bristol (Lead), Monash University, University College Dublin, University of Granada.
Work package 4 will develop and deliver two training systems: 1) A training system for healthcare staff to implement the GDM screening tool within EU sites; 2) A health coaching training programme for working with women during their infants’ first 1,000 days. Recruitment of health coaches and evaluation of the intervention delivery are also included in WP4.
Partners involved: University of Copenhagen (Lead), Liva Healthcare, North Bristol NHS Trust, University College Dublin, University of Bristol, University of Granada.
This work package will initiate the randomised controlled trial, ensuring it runs according to best ethical and trial procedures. The trial will begin at the Dublin site and will be subsequently rolled out across the other country sites in the UK, Spain and Australia. This will ensure maximum learning amongst sites.
Partners involved: University of Copenhagen (Lead), Liva Healthcare, Monash University, North Bristol NHS Trust, University College Dublin, University of Bristol, University of Granada.
Work package 6 will drive the analysis plans and integration of findings into dissemination activities (WP8). It includes developing strategies for the analysis of outcomes, cost-effectiveness, data, and factors associated with the success of the intervention. It will also evaluate the results of the statistical analyses and the cost-effectiveness analysis, comparing results across settings.
Partners involved: University College Dublin (Lead), Aarhus University, Beta Technology, Deakin University, Liva Healthcare, Monash University, University of Bristol, University of Copenhagen, University of Granada.
The aim of work package 7 is to ensure timely, effective and successful delivery of the project by providing a high level of administrative, contractual, financial and managerial support. The project is coordinated by Dr Sharleen O’Reilly from University College Dublin and supported by all partners.
Work package 8 will ensure that the outcomes and achievements from the project are effectively transferred to end users and there is measurable uptake. This includes promotion of the project and its activities and results to a wide range of stakeholders, enabling knowledge transfer and innovation and maximising the project’s impacts. An implementation forum will be set up to guide and facilitate engagement with policymakers and healthcare decision makers throughout the project.
WP8 is led by Beta, supported by UCD and all other project partners.
Work package 9 is responsible for monitoring the ethics and data privacy for the project. It will ensure that it follows the necessary criteria and procedures for ethics and the data is GDPR compliant. The ethics work package receives external and independent advice from the project’s External Advisory Board.
This work package is led by University College Dublin.
What previous research is the project based on?
The project will take the evidence outlined below and synthesise it to create an innovative and unique approach to managing weight management in pregnancy and the first year of life to ensure both mother and baby have a healthy pregnancy and the best start in life.
| Evidence | Detail | Link to publication |
|---|---|---|
| Monash GDM Screening Tool, 2011 | 4,276 women attending a large tertiary hospital were screened using risk factors for GDM easily identified at the first-trimester midwifery hospital booking visit. This risk prediction tool identified women at high risk of GDM and represents a novel approach to facilitate targeted early intervention. | |
| Pregnancy Exercise, nutrition with App support Research Study (PEARS), 2015-2017 | PEARS was a lifestyle intervention versus usual care in women with BMI > 25kg/m2. The intervention focused on a low diet and exercise grounded in behaviour theory delivered using an individual session and a phone app. Whilst the trial did not reduce GDM, there were significant differences in reduced gestational weight gain and lower rates of large gestational age infants in those using the intervention. | |
| InFANT and My Baby Now | A trial delivered for children aged 3-18 months through first-time pregnancy groups. The trial significantly improved energy-balance behaviours in mothers and children at 18 month and 5 year follow ups. Mothers and children both experienced healthier behaviours including eating more vegetables, eating fewer sugary snacks and greater dietary knowledge. The trial confirmed the hypothesis that early childhood interventions could have significant and meaningful change in child BMI. | |
| The Mothers After Gestational Diabetes in Australia (MAGDA); 2011-2016 | The study was a key component of the first and only systematic approach in the world aiming to prevent conversation from GDM to type-2 diabetes. The lifestyle intervention consisted of a single individual session, five group sessions and two follow-up phone calls, and resulted in an average 1kg difference between control and intervention groups. The weight difference is effective at reducing GDM and other long-term negative effects on the offspring. MAGDA also developed the programme further to address barriers to physical attendance by integrating health coaching and an app delivery. The programme has had significant effects on Australian policy and practice. | |
| Healthy Lifestyle Programme (HeLP-her) Intervention | A low intensity intervention, integrated with standard antenatal care is effective in limiting postpartum weight retention. |


 Implementation Toolkit
Implementation Toolkit