From design to data: Understanding the tools of health research
Blog by Kate Wall and Sharleen O’Reilly
Let’s imagine you’re a researcher wanting to explore the impact of a new health behaviour change programme for pregnant or post-partum women. What tools would you use to measure success? How would you ensure your results are reliable and meaningful?
In this blog, we’ll walk through the key components of health research, from designing your study to collecting and interpreting data. Starting at the very beginning, we need to understand some key terms and how a study is constructed.
Designing a trial
Randomised controlled trials (RCTs) are a type of scientific experiment used to compare the impact of an intervention on two or more groups. RCTs have an experimental group (which receives the intervention) and a control group (which doesn’t). This setup helps researchers examine the cause-and-effect relationship between the intervention and the outcome.
Researchers measure outcomes in both groups at specific times throughout the study. They then analyse the differences between the groups statistically. By randomly assigning participants to these groups, researchers reduce bias. This randomisation helps balance participant characteristics across groups, allowing any differences to be attributed to the study intervention.
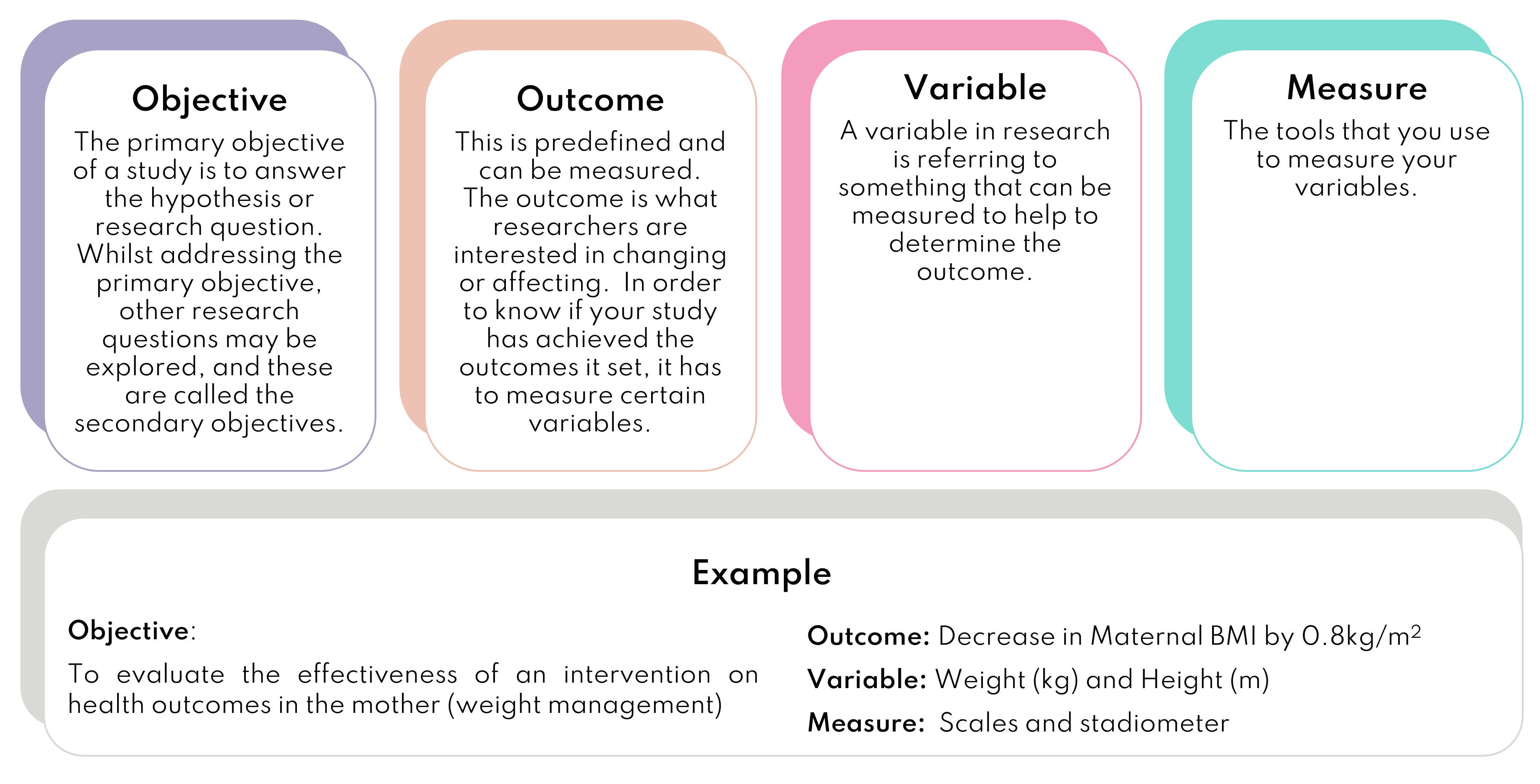
Every research study has expected outcomes – changes that should happen because of the intervention being tested. These outcomes align with the study’s main goal or aim.
The primary outcome is the main event that the study is designed to assess. It’s the variable most likely to answer the main research question. Secondary outcomes help interpret the primary outcome results. They’re often more exploratory and may spark ideas for future research.
The Bump2Baby and Me trial aimed to test an intervention supporting women’s weight management during pregnancy and for 12 months after birth. The primary outcome was a reduction in maternal body mass index (weight in kg divided by height in metres squared) in the intervention group. Secondary outcomes included maternal blood pressure, metabolic markers, diet, blood glucose levels and gestational diabetes diagnosis.
These kinds of outcomes are common in health research, so let’s take a closer look at some of the methods researchers can use to measure these.
What you measure matters!
In health-related research, we use both objective and subjective measures to assess outcomes. Objective measures provide unbiased, reliable data, while subjective measures offer insight into participants’ lived experiences.
Baseline measurements, taken before the intervention begins, are critical in well-designed intervention studies. They provide a reference point for any subsequent changes or actions to evaluate subsequent changes.
Objective measures
These are tools that can measure consistently and accurately such as blood tests. Another set of measurements that are objective are anthropometry, which is measurement of the body’s different physical properties such as height, weight and waist circumference.
Body Mass Index (BMI)
Height and weight are used together to calculate BMI. BMI is used to determine if a person is in the healthy weight category (18.5-24.9) based on population distributions of both weight and height. There are 5 BMI classifications from underweight (<18.5), overweight (25-29.9) to morbid obesity (>35.0). BMI is useful when looking at the effectiveness of interventions on public health because it is based on large-scale population research and is quick, cheap, non-invasive and reproducible.
BMI does have limitations – it doesn’t tell you anything about where body fat is distributed; individuals with similar BMIs may not have the same amount of fat in their body, and the fat can be distributed differently, leading to different health outcomes1. This limitation means BMI is usually only part of the picture when screening for health status. BMI is commonly used in obesity studies2 as well as studies on other metabolic diseases such as type 2 diabetes3 (particularly in women4) and gestational diabetes5. This is because people with a BMI over 30 have a higher risk of dying or having serious health events6. BMIs over 30 are also predictive of having a higher body fat level and obesity7. When combining all these factors, if BMI is measured correctly, it is a useful marker to identify health status.
Metabolic health markers
Metabolic health markers tend to look at body fat distribution (waist and hip circumference), blood pressure and the levels of fat (high-density cholesterol and triglycerides) and glucose in the blood. These health markers point to whether someone has metabolic syndrome or not. If someone has three or more of these markers, they would be diagnosed with metabolic syndrome8 and individually, these indicate an issue with metabolic health.
The biomarkers found in blood, such as cholesterol, triglycerides, glucose, and blood pressure provide high-quality measures of what is happening inside the body in relation to someone’s health. They are normally measured at the start of an RCT as baseline measurements; researchers can compare the results over time and use them to test if an intervention changes people’s metabolic health. The values can also be compared with the wider population to see how well those involved in the trial compare with an average person.
Subjective measures
These tools capture what people say or feel, like scales and questionnaires.
Food frequency questionnaires (FFQs)
FFQs are a key research tool to explore what people are eating. They are designed to capture how often and how much food is eaten over time. This information can help to explore the link between a person’s average diet over a specific time, e.g., one month, and health outcomes, such as obesity or diabetes. By looking at a longer-term snapshot of the foods someone eats, researchers can see if the person eats a high or low amount of that food or nutrient. They can then study other risk factors to see if they are also high or low and use this information to check if there may be an association between the dietary pattern and different diseases.
FFQs include the main foods that contribute to the nutrients or dietary patterns the research team is interested in. For example, foods with different levels of sugar and fibre such as fruits, vegetables, breads and sweets would be important to check if you were interested in studying gestational diabetes.
Example portion size and question from an FFQ
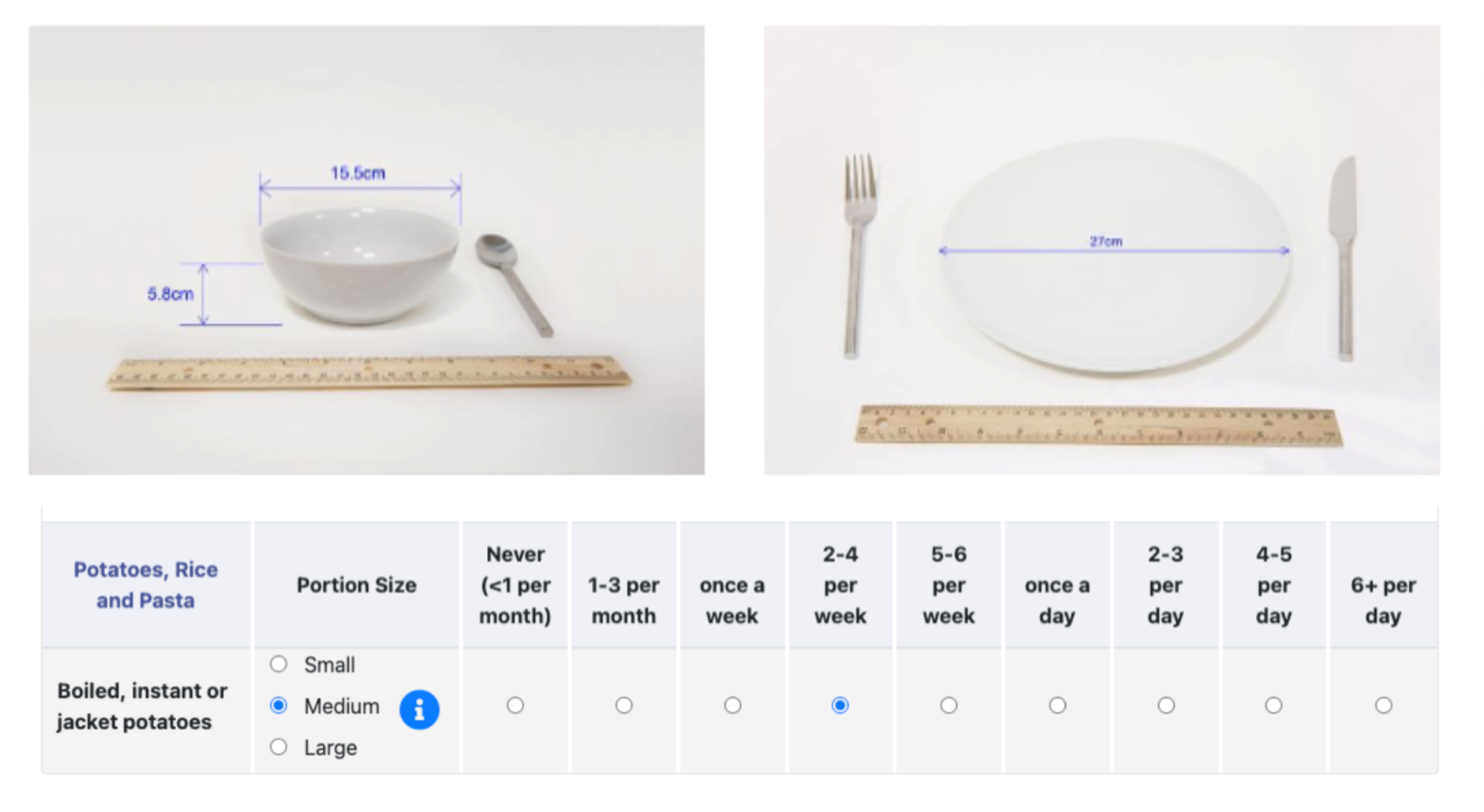
Because diets vary between countries, it is important to use an FFQ validated or checked against the diet in the country where the research is being done. For example, the Food4Me questionnaire9 used in the Bump2Baby and Me trial was checked using populations in the UK, Ireland, Spain and several other European countries. The checks look to see how different the nutrient or food levels are between the FFQ and another diet assessment tool like food diaries.
Health literacy questionnaires
A person’s health literacy can determine how well they can manage their health and understand and use the right health services10. It is defined as the ‘ability to make sound health decisions in the context of everyday life – at home, in the community, at the workplace, the healthcare system, the marketplace and the political arena’11. Low health literacy is linked to higher chances of dying12, lower use of healthcare13 and lower ability to manage diseases such as diabetes14.
The Bump2Baby and Me study strives to support women’s health literacy. We included this important measure using the health literacy questionnaire, a validated tool10 shown to be robust in populations at risk of metabolic disease15.
Exit interviews
Interviews allow researchers to gather rich qualitative data to enhance the other information collected during the trial16. This type of data provides deeper information about the participant’s experience, feelings, and social setting, which is not possible through numbers17. They can give a much fuller understanding of what the trial has achieved and its impact.
Summary
We can see how each tool and method in behaviour change research plays a key role in uncovering valuable insights. From the initial design of an RCT to the final analysis of both objective and subjective data, every step contributes to our understanding of the health intervention. Our researcher, armed with BMI measurements, metabolic markers, food frequency questionnaires, and health literacy assessments, is now well-equipped to evaluate the effectiveness of the weight management programme for pregnant women.
These diverse tools allow us to paint a comprehensive picture of participants’ health, capturing not only physical changes but also shifts in behaviour and understanding. By combining rigorous scientific methods with tools that measure lived experiences, we create research that is both robust and relevant to real-world health challenges. As we continue to refine these methods and develop new ones, we move ever closer to our goal of improving health outcomes for individuals and communities alike. Remember, behind every health recommendation and policy lies a wealth of careful research, employing the tools and techniques explored in this blog.
References
- Wolfe RR. The underappreciated role of muscle in health and disease. Am J Clin Nutr. 2006;84(3):475–82.
- Sweatt, K., Garvey, W.T. & Martins, C. Strengths and Limitations of BMI in the Diagnosis of Obesity: What is the Path Forward?. Curr Obes Rep (2024). https://doi.org/10.1007/s13679-024-00580-1
- Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89(3):309–19.
- Sommer, I., Teufer, B., Szelag, M. et al. The performance of anthropometric tools to determine obesity: a systematic review and meta-analysis. Sci Rep 10, 12699 (2020). https://doi.org/10.1038/s41598-020-69498-7
- Torloni MR, Betran AP, Horta BL, Nakamura MU, Atallah AN, Moron AF, et al. Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta-analysis. Obes Rev. 2009;10(2):194–203.
- Flegal, K. M., Kit, B. K., Orpana, H. & Graubard, B. I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 309, 71–82. https://doi.org/10.1001/jama.2012.113905 (2013).
- Romero-Corral, A., Somers, V. K., Sierra-Johnson, J., Thomas, R. J., Collazo-Clavell, M. L., Korinek, J., Allison, T. G., Batsis, J. A., Sert-Kuniyoshi, F. H., & Lopez-Jimenez, F. (2008). Accuracy of body mass index in diagnosing obesity in the adult general population. International journal of obesity (2005), 32(6), 959–966. https://doi.org/10.1038/ijo.2008.11
- American Heart Association (2023) What is metabolic syndrome? [Online] https://www.heart.org/en/health-topics/metabolic-syndrome/about-metabolic-syndrome. Accessed July 2024
- Forster, H., Fallaize, R., Gallagher, C., O’Donovan, C. B., Woolhead, C., Walsh, M. C., … & Gibney, E. R. (2014). Online dietary intake estimation: the Food4Me food frequency questionnaire. Journal of medical Internet research, 16(6), e3105.
- Osborne, R. H., Batterham, R. W., Elsworth, G. R., Hawkins, M., & Buchbinder, R. (2013). The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC public health, 13, 1-17.
- Kickbusch, I., Wait, S., & Maag, D. (2005). Navigating health: The role of health literacy.
- Peterson PN, Shetterly SM, Clarke CL, Allen LA, Matlock DD, Magid DJ, Masoudi FA: Low Health Literacy is Associated With Increased Risk of Mortality in Patients With Heart Failure. Circulation 2009, 120(18):S749–S749.
- Scott TL, Gazmararian JA, Williams MV, Baker DW: Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Medical Care 2002, 40(5):395–404.
- Marciano, L., Camerini, A. L., & Schulz, P. J. (2019). The role of health literacy in diabetes knowledge, self-care, and glycemic control: a meta-analysis. Journal of general internal medicine, 34, 1007-1017.
- Debussche, X., Lenclume, V., Balcou-Debussche, M., Alakian, D., Sokolowsky, C., Ballet, D., … & Huiart, L. (2018). Characterisation of health literacy strengths and weaknesses among people at metabolic and cardiovascular risk: Validity testing of the Health Literacy Questionnaire. SAGE open medicine, 6, 2050312118801250.
- Higgs J, Titchen A. Propositional, professional and personal knowledge in clinical reasoning. In: Higgs J, Jones M, eds. Clinical reasoning in the health professions . Oxford: Butterworth-Heinemann, 1995; 129–146.
- National Health and Medical Research Council. Ethical aspects of qualitative methods in health research. An information paper for institutional ethics committees. Canberra: Australian Government Publishing Service, 1995.
- The Full story Education Team (2021). Qualitative vs. quantitative data in research: what’s the difference? [Online] https://www.fullstory.com/blog/qualitative-vs-quantitative-data/ Accessed July 2024.