mHealth: Shaping the future of maternity care
The final Bump2Baby and Me forum “Engaging with mHealth: Shaping the Future of Maternity Care” took place on Wednesday 20th November 2024. The forum provided an update on some of the sub-studies from the project. It also encouraged the sharing of best practices by bringing together academics, intermediaries and healthcare representatives from across the globe.
At the heart of the forum’s discussion was the concept of mHealth – leveraging mobile technologies like smartphones and apps to enhance healthcare delivery, improve patient outcomes, and advance health-related research. The Bump2Baby and Me project has developed and tested an mHealth intervention using an app and health coaching programme to help prevent maternal and child diabetes, overweight and obesity and other non-communicable associated diseases.
Latest from the project
Opening the forum, Professor Sharleen O’Reilly, Project Coordinator and Associate Professor at University College Dublin, explained the background to the project and the latest project developments. Statistics around gestational diabetes, a condition of pregnancy which can cause both short and long-term implications for both the mother and her child, show that, for example, approximately 50% of women who have gestational diabetes will develop type 2 diabetes within 5–10 years.
In the Bump2Baby and Me randomised controlled trial, women were screened in early pregnancy using a risk assessment tool at their first antenatal visit. Women at high risk of developing gestational diabetes, and who agreed to participate, were randomised to usual care or usual care plus the Bump2Baby and Me mHealth coaching programme. The trial took place in Ireland, Spain, UK and Australia and provided women with evidence-based healthy eating and exercise information, both during pregnancy and for the first year after birth, via a smartphone app and real-life health coach.
During the trial, data was collected on maternal and birth outcomes, gestational diabetes diagnosis, weight, diet, exercise and sleep, as well as other health metrics for mothers and babies. The trial had a 72% retention rate which is high for a long intervention and about half of eligible women chose to participate.
Understanding current practices
Professor Christy Burden, Associate Professor in Obstetrics at the University of Bristol and the Bump2Baby and Me UK Clinical Lead, explained that the project sought to understand current practices for screening, diagnosis and care of women once they were diagnosed with gestational diabetes and how it differed across the countries taking part in the trial.
Back in 2021, the project undertook a cross-sectional online survey. The aim was to find out what screening and diagnostic guidelines they used, what risk factors were used for screening and what care was currently provided to women. And, because this was undertaken at the time of the COVID pandemic they also asked if there were any changes to care practices due to this.
From the responses, it was clear there were variances in screening, testing and diagnosis, as well as in the use of national guidelines. COVID also exacerbated these differences, increasing the reliance on local or pandemic-specific guidelines. The survey underscores a significant variation in GDM care practices across the globe and highlights a huge postcode lottery which creates inequities in care and outcomes. mHealth holds promise as a solution to provide more consistent, standardised care throughout the pregnancy journey, potentially transforming gestational diabetes management globally.
Engagement in mHealth
Signe Boldt Bendsen, a Research Scientist from Liva Healthcare, explained her research which looked at how 300 participants in the intervention group of the Bump2Baby and Me randomised controlled trial interacted with the mHealth coaching app during pregnancy and through their child’s first year.
The goal was to analyse engagement patterns within the app, focusing on how participants used various features and interacted with their coach. Key features of the app included personalised coaching, learning materials and group chats.
Overall, it showed the human coaching element was critical, as most participants relied on it more than other app features and the more engaged they were, the less likely they were to drop out of the trial. Signe suggested that further research could explore connections between the different engagement types, e.g., those who are more engaged with the app rather than the coaching interactions, and health outcomes such as gestational diabetes prevention.
Enhancing breastfeeding confidence
Liz McGovern, Lactation Consultant and PhD Student at University College Dublin, explained the findings from her scoping review on breastfeeding and self-efficacy. This focused on prenatal interventions to improve breastfeeding outcomes emphasising the importance of self-efficacy, theoretical frameworks, and timing in intervention design.
Liz discussed the importance of self-efficacy in breastfeeding and the factors affecting this self-belief, including knowledge, attitudes, past experiences, and the influence of peers, family and healthcare professionals. The prenatal period is under-researched but critical for building confidence before the challenges of postnatal life arise. Early intervention during pregnancy allows more time to embed confidence and skills. The scoping review mapped existing research on prenatal breastfeeding self-efficacy to analyse theoretical frameworks, measurements, interventions, and their impact on outcomes.
The review found that out of 184 studies, 84 focused on interventions, mostly starting in the third trimester; earlier prenatal interventions remain rare. Previous effective components of interventions such as observing others breastfeeding, encouragement from healthcare professionals and personal networks all contributed towards a high self-efficacy. Lessons for designing interventions included: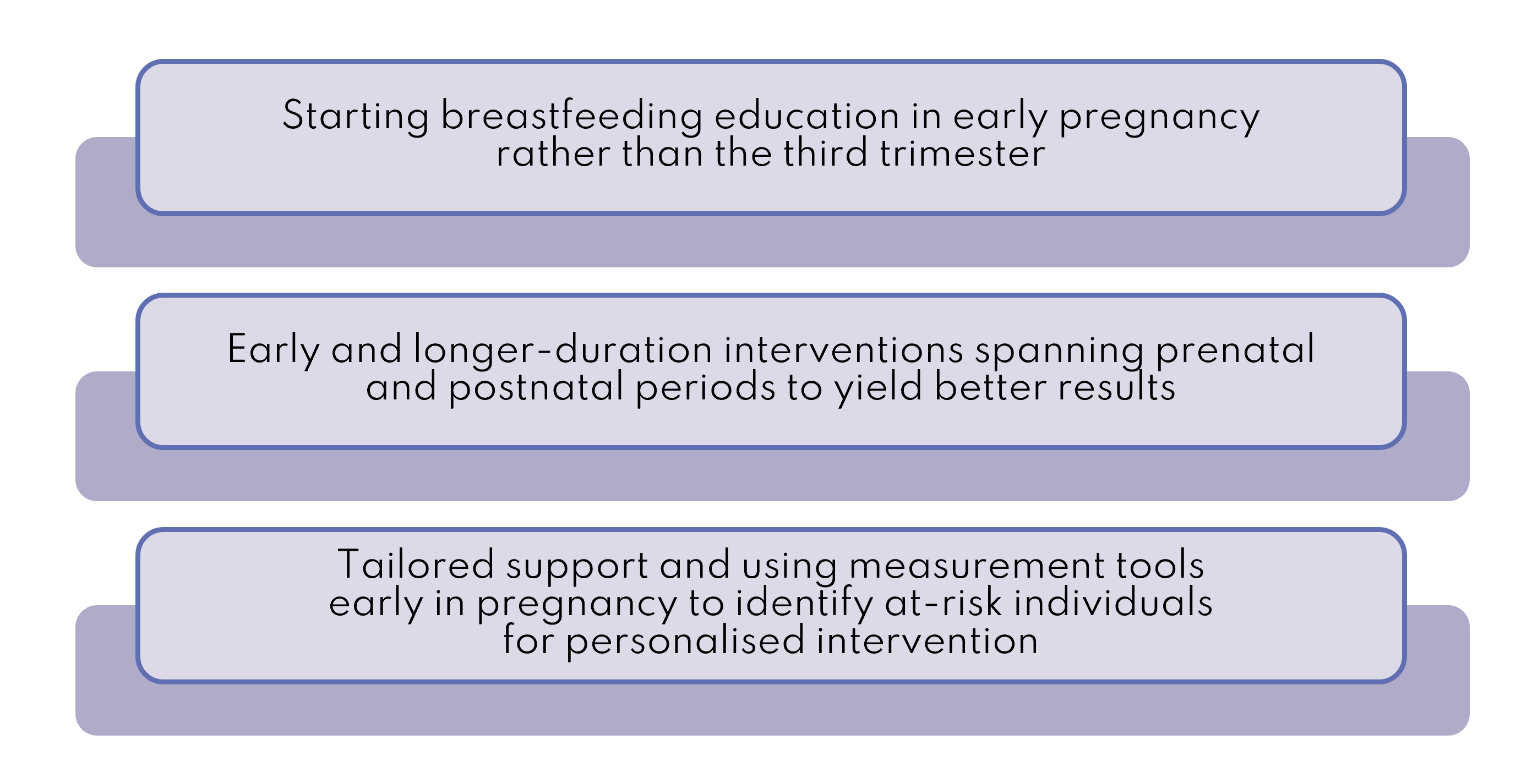
Going forward mHealth interventions should leverage theoretical models, early measurement tools, and sustained engagement across both prenatal and postnatal periods.
Next steps for the project
As the project nears the end, the baseline publication which focuses on the characteristics of the at-risk population is under review and the primary outcomes paper is in preparation. The Implementation Toolkit (resources and tools for healthcare professionals and policymakers) is expected in the first half of 2025. Starting from March 2025, the project results and lessons learnt will be disseminated at a series of implementation workshops across the participating countries. To register your interest please contact Kate Wall.
A recording of the forum is available below.
References
1.Centers for Disease Control and Prevention https://www.cdc.gov/diabetes/basics/gestational.html
2.Tommy’s, https://www.tommys.org/pregnancy-information/pregnancy-complications/gestational-diabetes/long-term-implications-gestational-diabetes