The importance of workforce factors in adopting new healthcare innovations
Healthcare innovations and new interventions to support patients can be really effective and often gather a lot of attention initially. However, uptake within existing systems and understanding how to make these interventions work in the real world and in the long term is vital.
The Health Service Executive (HSE) Spark Summit is a healthcare innovation conference in Ireland which provides an opportunity for healthcare professionals and academics to showcase their creativity and innovative thinking to improve healthcare for all. The annual summit showcases projects which aim to improve patient experiences, by harnessing healthcare professionals’ knowledge to bridge gaps in healthcare provision and build more flexible, resourceful, and efficient methods of care. This year’s Spark Summit was hosted in Dublin on 16th June 2022. A key take away from the conference was that it takes a wide group of people to effect change.
Some of the Bump2Baby and Me team in Dublin were delighted to attend and present at the conference. Nessa Cooney, a third year undergradute student from UCD, completed a 10 month placement with the Bump2Baby and Me study in 2022. Her project was presented as a poster at the summit (snapshot below).
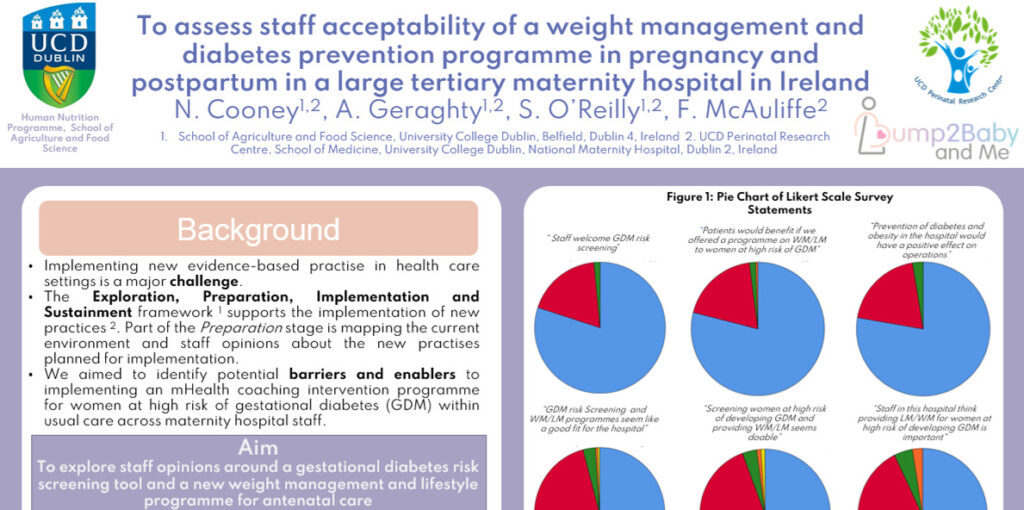
She presented under the theme ‘Importance of Design’ and reinforced the theory that creative thinking and careful evaluation is vital when implementing interventions and new evidence-based practice in healthcare settings. Research shows that it is important that staff support new interventions and that there is consensus among staff, management, and stakeholders in relation to introducing and implementing new programmes.
What did we find?
Nessa’s project consisted of a staff survey in Dublin’s National Maternity Hospital, one of the four Bump2Baby and Me trial sites. 195 staff completed the survey about risk screening for gestational diabetes and lifestyle and weight management programmes for patients.
Overall, hospital staff were supportive of these initiatives. More patient-facing staff agreed with patients benefiting from these programmes and with them being doable in the current clinical setting, compared to non-patient facing staff. Experience level impacted opinions with long-term staff (more than 15 years experience) reporting less confidence that risk screening would be welcomed in the hospital. However, they also reported feeling that other staff would be motivated to provide the programmes, and hospital leadership would be supportive.
This research indicates that the acceptability of new hospital practices may be influenced by staff factors such as experience levels and patient engagement levels. Therefore, workforce factors should be considered when preparing to adopt new antenatal lifestyle programmes. The findings might be useful in helping to inform the ongoing global conversation regarding the deployment of new antenatal programmes, as well as helping implementation of new programmes in other areas of healthcare. We hope to build on this work within the Bump2Baby and Me project over the coming months.