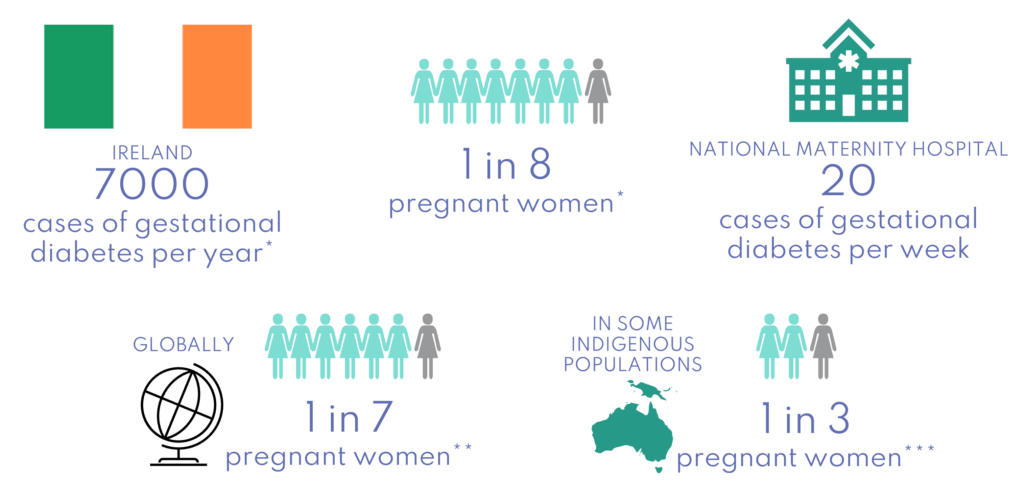
Gestational diabetes: a growing burden and a challenge
Gestational diabetes health risks
Gestational diabetes is the most frequent complication experienced during pregnancy. It is also a leading cause of maternal mortality and results in higher maternal health complications such as preeclampsia, macrosomia, birth difficulties, caesarean section, still birth, premature labour, neonatal hypoglycaemia, and admissions into neonatal intensive care, as well as causing additional stress around the time of birth.
Having gestational diabetes is also a flag for future type 2 diabetes risk in these women and their children. One in two women with gestational diabetes will develop type 2 diabetes within 5-10 years after birth.1 More recent data suggests this risk may be even higher with women who have had previous gestational diabetes having an 8-fold risk compared with a woman with no diabetes in pregnancy.2 This means that gestational diabetes is a huge burden for the mother, her baby, and the health system – and rates continue to rise.
Experiences are varied
For most women, being diagnosed with gestational diabetes comes out of the blue. In some countries, the initial stress of diagnosis is compounded by an additional financial stress caused by the out-of-pocket costs of regular fingerprick glucose testing. In Ireland, the cost is about €300 and for some women, it can mean the difference between them engaging or not engaging with proper healthcare.
Screening for gestational diabetes is another procedure that varies from country to country – even between hospitals within the same country! There is often an urban-rural divide for screening, which means that some women have significant travel and increased inconvenience associated with attending their screening appointments, which can be a real barrier.
Finally, we are all aware that COVID-19 created big challenges in healthcare delivery, and screening for gestational diabetes was also impacted with lots of services moving to quicker but less accurate tests for peak social distancing restrictions. The restrictions did however bring about some positives in the area of remote and mobile healthcare delivery.3 For example, some gestational diabetes clinics moved to fingerprick glucose testing that could be tracked on a mobile app and sent through securely for the team to review. This has greatly improved the woman’s experience and helped her healthcare team see up-to-date and accurate information at her virtual visit.
Focus on prevention
Pregnancy is a window of opportunity. During this time, we can establish health services, improve the health of mums, and create lasting relationships with women that will allow us to help prevent intergenerational transmission of non-communicable diseases.
Given the link between gestational diabetes, poor pregnancy outcomes and the future risk of chronic disease – prevention needs to be our focus. Screening and early diagnosis, as well as the good management of gestational diabetes, are key to improving outcomes for all women.
Family-centric interventions are also key and previous evidence has shown that lifestyle modification as a treatment is effective in the postpartum period. For example, the US Diabetes Prevention Programme had a 58% reduction in risk after one year and this risk was still reduced ten years afterwards (35% lower).4 5 The evidence shows that diet alone and the combination of both diet and exercise interventions in pregnancy and postpartum are cost-effective.6 7 In addition, digital interventions are welcomed by women with gestational diabetes.8
Bump2Baby and Me Trial
This and other evidence led to the creation of the Bump2Baby and Me trial. We are testing an innovative healthcare intervention which provides women with evidence-based healthy eating and exercise information, both during pregnancy and for the first year after birth, via a smartphone app and real-life health coach. The trial focuses on working with women who are identified at high risk of gestational diabetes and who will therefore benefit most from this behaviour change intervention. To do this we are using the Monash Gestational Diabetes Risk Screening Tool. Commonly collected data from the first antenatal appointment is used to calculate a score which gives us a good indication of future risk.9
 We have recruited almost 800 women and 85 babies have been born. These women will participate until their babies are one year old, at which time we will begin analysis of the data collected.
We have recruited almost 800 women and 85 babies have been born. These women will participate until their babies are one year old, at which time we will begin analysis of the data collected.
Gestational diabetes was the topic of our recent policy forum which brought together policy and health stakeholders for an interactive discussion. You can connect with us via these regular forums. The next one will take place on 6th April 2022. You can also follow us on Twitter and LinkedIn.
Infographic References
*O’Sullivan, E.P., Avalos, G., O’Reilly, M. et al. Atlantic Diabetes in Pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 54, 1670–1675 (2011).
**IDF Diabetes Atlas 10th Edition (2021).
***Voaklander B, et al. Prevalence of diabetes in pregnancy among Indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta-analysis. The Lancet Global Health, 8(5), E681-E698 (2020).
Text References
1Kim, C., Newton, K., & Knopp, R. (2002). Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care, 25(10), 1862-1868.
2Dennison, R. A., Chen, E. S., Green, M. E., Legard, C., Kotecha, D., Farmer, G., Sharp, S. J., Ward, R. J., Usher-Smith, J. A., & Griffin, S. J. (2021). The absolute and relative risk of type 2 diabetes after gestational diabetes: A systematic review and meta-analysis of 129 studies. Diabetes Research and Clinical Practice, 171, 108625.
3Varnfield M, Redd C, Stoney RM, et al. M♡THer, an mHealth System to Support Women with Gestational Diabetes Mellitus: Feasibility and Acceptability Study. Diabetes Technol Ther. 2021;23(5):358-366.
4Ratner, R. E., Christophi, C. A., Metzger, B. E., Dabelea, D., Bennett, P. H., Pi-Sunyer, X., Fowler, S., Kahn, S. E., & The Diabetes Prevention Program Research Group. (2008). Prevention of Diabetes in Women with a History of Gestational Diabetes: Effects of Metformin and Lifestyle Interventions. J Clin Endocrinol Metab, 93(12), 4774-4779.
5Aroda, V. R., Christophi, C. A., Edelstein, S. L., Zhang, P., Herman, W. H., Barrett-Connor, E., Delahanty, L. M., Montez, M. G., Ackermann, R. T., Zhuo, X., Knowler, W. C., & Ratner, R. E. (2015). The Effect of Lifestyle Intervention and Metformin on Preventing or Delaying Diabetes Among Women With and Without Gestational Diabetes: The Diabetes Prevention Program Outcomes Study 10-Year Follow-Up. The Journal of Clinical Endocrinology & Metabolism, 100(4), 1646-1653.
6Bailey, C., Skouteris, H., Harrison, C. L., Boyle, J., Bartlett, R., Hill, B., Thangaratinam, S., Teede, H., & Ademi, Z. (2020). Cost Effectiveness of Antenatal Lifestyle Interventions for Preventing Gestational Diabetes and Hypertensive Disease in Pregnancy. PharmacoEconomics – open, 4(3), 499–510.
7Bailey, C., Skouteris, H., Teede, H. et al. Are Lifestyle Interventions to Reduce Excessive Gestational Weight Gain Cost Effective? A Systematic Review. Curr Diab Rep 20, 6 (2020).
8Niamh Kelly-Whyte, Ciara McNulty, Sharleen O’Reilly, Perspectives on mHealth Interventions During and After Gestational Diabetes, Current Developments in Nutrition, Volume 5, Issue Supplement_2, June 2021, Page 768.
9Teede, H. J., Harrison, C. L., Teh, W. T., Paul, E., & Allan, C. A. (2011). Gestational diabetes: development of an early risk prediction tool to facilitate opportunities for prevention. Aust N Z J Obstet Gynaecol, 51(6), 499-504.