Women’s belief in their ability to breastfeed influences outcomes
In this blog post from Liz McGovern, Lactation Consultant and University College Dublin (UCD) PhD Student in the Bump2Baby and Me Project, she explains the importance of breastfeeding confidence / self-efficacy and how increasing it supports women to breastfeed for longer and more exclusively. She outlines her work exploring this concept in the antenatal period and her analysis of the infant feeding information provided by Bump2Baby and Me families across the project.
Breastfeeding is the process by which human breastmilk is fed to a child, whether by feeding directly at the breast (also referred to as chestfeeding for inclusivity) or by pumping milk and feeding by bottle (sometimes called breastmilk feeding if exclusively done this way). Breastmilk is nutritionally complete and is tailored to the needs of the baby, for example a premature baby will receive milk that is higher in energy, fat, protein and immune factors to meet their needs and development. Breastmilk provides health protection in the short and long term for both the baby and their nursing parent and has even been referred to as personalised medicine for babies. It protects children from infections, particularly ear and respiratory tract infections and gastroenteritis, and can lower their risk of diseases such as diabetes, childhood leukaemia, asthma, overweight/obesity and atopic dermatitis. Breastfeeding also lowers mothers’ risks of breast and ovarian cancers, type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular disease.
Breastfeeding guidelines
For optimum growth, development and health of infants and children, the World Health Organisation (WHO) and the United Nations Children’s Fund (UNICEF) jointly recommend that babies should be exclusively breastfed for their first 6 months, followed by continued breastfeeding alongside nutritious, complementary food for up to 2 years and beyond. However, breastfeeding rates are nowhere near these recommendations, with only 44% of the world’s children being breastfed exclusively for 6 months.
Factors which influence breastfeeding
There are many factors that contribute to decisions around breastfeeding. Some are considered to be fixed or non-modifiable like geographical location, maternal age, number of children, and socioeconomic, marital and educational status. There are other factors that have been shown to contribute to breastfeeding initiation, duration and exclusivity and can be influenced or modified, such as the type of birth experienced, previous breastfeeding experience, knowledge of the benefits of breastfeeding, attitudes to infant feeding, confidence (self-efficacy) in breastfeeding, and social and professional support received.

Mum breastfeeding with support from dad
Breastfeeding self-efficacy
Self-efficacy refers to a person’s belief in their ability to either complete a task or reach a goal. The psychologist, Albert Bandura, hypothesised in 1977 in his paper on self-efficacy that it has a direct influence not only on the motivation to initiate a behaviour, but also on the effort expended and level of coping in the face of obstacles. He based this on the understanding that people will avoid situations and activities that they believe are beyond their coping skills, and get involved assuredly and persevere, when they feel that they have the ability to succeed.
Lactation consultant Cindy-Lee Dennis applied Bandura’s self-efficacy theory to breastfeeding, describing it as the self-belief and confidence a woman has in her perceived ability to breastfeed. It is a strong modifiable predictor of breastfeeding outcomes and can identify people at higher risk of breastfeeding cessation. Studies show that mothers with high levels of breastfeeding self-efficacy in the postnatal period are more likely to be breastfeeding at key postnatal timepoints than those with lower levels.
Many things contribute to a person’s breastfeeding self-efficacy, including their knowledge, attitudes, previous experiences, the views of important people in their lives (partner, family, friends), support they receive, societal norms, and seeing others breastfeed. Breastfeeding self-efficacy theory advocates the inclusion of these factors, but interventions often only focus on enhancing education. The timing of interventions to improve self-efficacy is also important. It develops over time, like any sense of confidence and competency, so improving it early could increase the impact on breastfeeding initiation as well as duration and exclusivity.
My research and work in Bump2Baby and Me
My PhD is focusing on prenatal breastfeeding self-efficacy and the related factors of infant feeding attitudes and intention. The first study is a scoping review of the literature to explore the evidence in the area, including identifying and describing the theoretical frameworks, measurements and interventions used and their impact on breastfeeding outcomes. The protocol for this review was published with Open Research Europe.
The Bump2Baby and Me randomised controlled trial (RCT) provides an opportunity to explore breastfeeding practices, through the lens of participant attitude and intention scores from the second trimester of pregnancy. These will be measured using the self-reported Iowa Infant Feeding Attitude Scale (IIFAS) and expression of feeding intention, which were collected via online questionnaire (12-20 weeks’ gestation).
The first year of my PhD was spent as an active member of the Dublin site team, screening and recruiting participants and assisting with data collection, alongside conducting a breastmilk substudy with Dublin participants, and preparing and publishing a plan for a scoping review of the literature. I conducted a breastmilk substudy where Dublin participants were invited to provide a small sample of their breastmilk when their baby was 6-8 weeks old. The aim of the substudy is to examine the impact of maternal metabolic and hormonal health on breastmilk composition in women at risk of gestational diabetes. I initially hoped that we would get samples from 50 women and was delighted when our final number of participants in the substudy was 107. I’d like to take this opportunity to thank them again for their wonderful cooperation and generosity in sharing their breastmilk with us. The samples are all safely in the deep freeze in UCD and will be analysed soon.
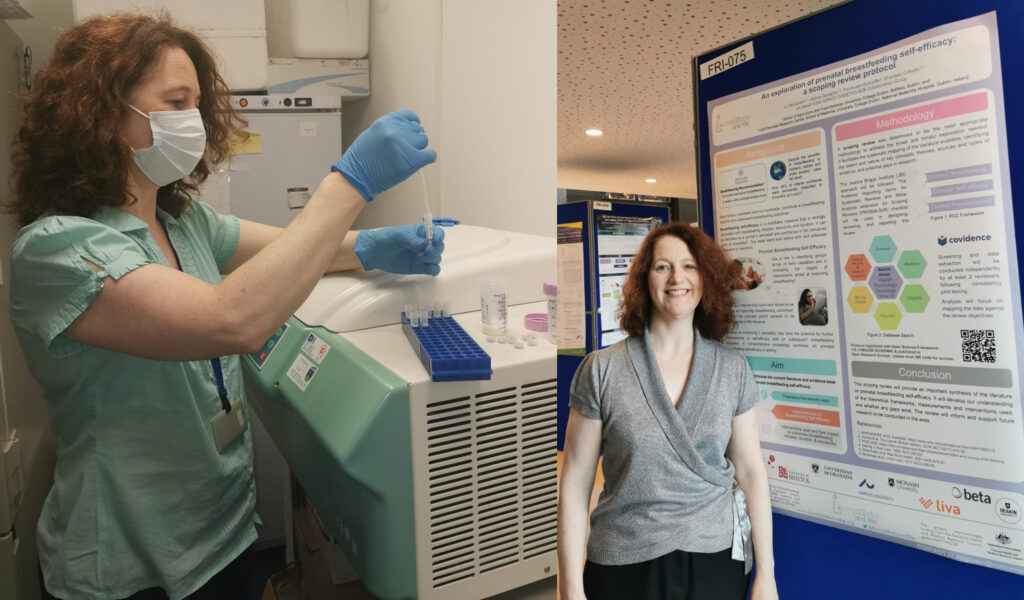
Liz preparing milk samples for the freezer and presenting her work at a conference
Over the next year, as the data becomes available from all study sites, I plan to analyse infant feeding practice of participants. I am interested in attitudes and intention for infant feeding expressed in early-mid pregnancy and exploring the relationship between these levels and breastfeeding initiation, exclusivity, and duration across the first year of their baby’s life. I also plan to include a study exploring feeding attitude and intention of Dublin participants and their willingness to participate in the breastmilk study.
I am looking forward to exploring the Bump2Baby and Me infant feeding practices across all sites and seeing whether prenatal attitudes and intention impacted the breastfeeding practice of participants. I hope that my work on prenatal breastfeeding self-efficacy will shine a light on the importance of focusing on the prenatal period. Ultimately, it would be wonderful to contribute to the increasing of breastfeeding rates through enhancing the understanding of prenatal breastfeeding self-efficacy.